Understanding Non-Small Cell Lung Carcinoma (NSCLC) Prognosis
Introduction
Non-small cell lung carcinoma NSCLC is one of the most common types of lung cancer, accounting for approximately 85% of all lung cancer cases. The prognosis for NSCLC can vary widely based on factors such as the stage at diagnosis, the patient’s overall health, and specific genetic mutations present in the cancer cells. This article delves into the details of NSCLC prognosis, including survival rates, treatment options, and factors that influence outcomes.
Overview of NSCLC
NSCLC can be further divided into several subtypes, with the most common being adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Each subtype has distinct histological and molecular characteristics, influencing the approach to treatment and prognosis.
Table 1: Subtypes of NSCLC and Their Characteristics
| Subtype | Description |
|---|---|
| Adenocarcinoma | Most common subtype; originates in glandular cells of the lung |
| Squamous Cell Carcinoma | Arises from the squamous cells lining the airways |
| Large Cell Carcinoma | Least common; characterized by large, abnormal-looking cells |
Prognostic Factors
The prognosis of NSCLC is influenced by a variety of factors, including:
- Stage at Diagnosis: Early-stage NSCLC has a significantly better prognosis compared to advanced stages.
- Genetic Mutations: Specific genetic alterations such as EGFR mutations or ALK rearrangements can affect prognosis and guide targeted therapy.
- Patient’s Overall Health: Comorbidities and overall fitness can impact treatment outcomes.
- Treatment Response: The effectiveness of initial treatment plays a critical role in prognosis.
Table 2: Survival Rates by Stage
| Stage | 5-Year Survival Rate (%) |
|---|---|
| Localized | 60-70% |
| Regional | 30-40% |
| Distant | 5-10% |
Staging of NSCLC
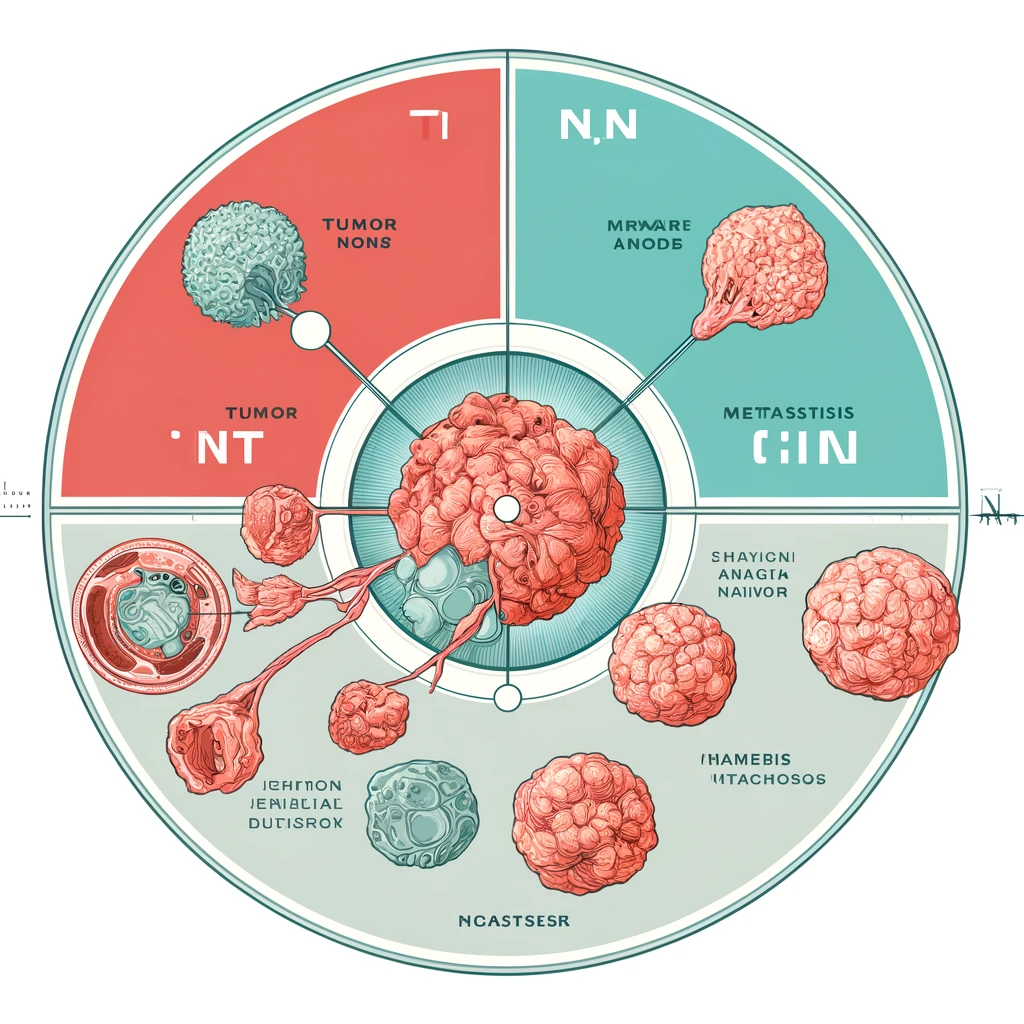
Staging is crucial in determining the prognosis and treatment strategy for NSCLC. The TNM staging system is commonly used, where:
- T (Tumor): Describes the size and extent of the primary tumor.
- N (Nodes): Indicates whether the cancer has spread to nearby lymph nodes.
- M (Metastasis): Refers to whether the cancer has spread to distant parts of the body.
Figure 1: TNM Staging System
Treatment Options
Treatment for NSCLC varies based on the stage and specific characteristics of the cancer. The main treatment modalities include:
- Surgery: Often the first-line treatment for early-stage NSCLC.
- Radiation Therapy: Used alone or in combination with other treatments for various stages.
- Chemotherapy: Commonly used for advanced stages or after surgery to eliminate residual cancer cells.
- Targeted Therapy: For cancers with specific genetic mutations.
- Immunotherapy: Emerging as a powerful option for advanced NSCLC.
Table 3: Treatment Modalities and Their Applications
| Treatment | Application |
|---|---|
| Surgery | Early-stage NSCLC |
| Radiation | Early to advanced stages, palliative care |
| Chemotherapy | Advanced stages, adjuvant therapy |
| Targeted Therapy | EGFR, ALK mutations, and other specific targets |
| Immunotherapy | Advanced stages, PD-L1 positive cancers |
Advances in Targeted Therapy and Immunotherapy
Recent advances in targeted therapy and immunotherapy have significantly improved the prognosis for certain subsets of NSCLC patients. Drugs targeting EGFR, ALK, ROS1, and other mutations have shown remarkable efficacy.
Table 4: Common Targeted Therapies for NSCLC
| Mutation Target | Drug Name | Response Rate (%) |
|---|---|---|
| EGFR | Erlotinib, Gefitinib | 60-70% |
| ALK | Crizotinib, Alectinib | 50-60% |
| ROS1 | Crizotinib | 70-80% |
Immunotherapy, particularly checkpoint inhibitors like pembrolizumab and nivolumab, has revolutionized the treatment landscape for NSCLC, providing durable responses in a subset of patients.
Figure 2: Mechanism of Action of Immunotherapy
Prognosis by Genetic Mutation
The presence of specific genetic mutations can significantly alter the prognosis and guide personalized treatment strategies. For instance, EGFR mutations are associated with a favorable response to tyrosine kinase inhibitors, while KRAS mutations often predict a poorer prognosis.
Table 5: Prognosis by Genetic Mutation
| Genetic Mutation | Prognosis | Treatment Implications |
|---|---|---|
| EGFR | Favorable with treatment | Targeted therapy with EGFR inhibitors |
| ALK | Favorable with treatment | ALK inhibitors |
| KRAS | Poorer prognosis | Limited targeted options, focus on immunotherapy |
Lifestyle and Supportive Care
Beyond medical treatments, lifestyle factors and supportive care play a critical role in the prognosis of NSCLC. Smoking cessation, nutritional support, and palliative care are essential components of comprehensive cancer care.
Table 6: Impact of Lifestyle Factors on NSCLC Prognosis
| Factor | Impact on Prognosis |
|---|---|
| Smoking Cessation | Improves overall survival |
| Nutritional Support | Enhances treatment tolerance |
| Physical Activity | Improves quality of life and outcomes |
Conclusion
The prognosis for NSCLC has improved significantly over the past decade, thanks to advances in targeted therapies and immunotherapy. Early detection remains crucial, as it significantly enhances the chances of successful treatment. Patients with specific genetic mutations can benefit from personalized therapies that offer improved survival rates. However, ongoing research and clinical trials are essential to further improve outcomes and discover new therapeutic targets.
Figure 3: Survival Improvement Over the Years
Embedded YouTube Video
Here is an informative video about recent advancements in NSCLC treatment:
References
- National Cancer Institute. (n.d.). Lung Cancer—Non-Small Cell.
- American Cancer Society. (2023). Non-Small Cell Lung Cancer Survival Rates.
- Healthline. (2024). Understanding Non-Small Cell Lung Carcinoma Prognosis.
This detailed article aims to provide comprehensive insights into the prognosis of NSCLC, backed by the latest research and clinical data.